Public Health is defined as “the art and science of preventing disease, prolonging life and promoting health through the organized efforts and informed choices of society, organizations, public and private, communities and individuals of society” (Acheson, 1988; WHO).
The focus of a public health intervention is to prevent and manage diseases, injuries and other health conditions through surveillance of cases and the promotion of healthy behaviors, communities and environments. Many diseases are preventable through simple, nonmedical methods. Public health focuses on the entire spectrum of health and wellbeing, not only the eradication of particular diseases. Many activities are targeted at populations such as health campaigns. Public health services also include the provision of personal services to individual persons, such as vaccinations, behavioural counselling, or health advice. Health" takes into account physical, mental and social well-being. It is not merely the absence of disease or infirmity, according to the World Health Organization.
Public health is interdisciplinary. For instance, disease control/epidemiology, nutrition, health promotion, health information/biostatistics, environmental health, mental health and public health nursing services are all relevant. Behavioural health, health economics, public policy, first aid and occupational safety are other important subfields.
FUNCTIONS OF PUBLIC HEALTH PROFESSIONALS
Public health professionals are trained to execute one or more of these crucial services:
1. Mobilze community partnerships to identify and solve health problems
2. Diagnose and investigate health problems and harzards in the community
3. Monitor the health status of a community to identify potential problems
4. Inform, educate, and empower people about health issues, particularly the underserved and those at risk
5. Develop policies and plans that support individual and community health efforts
6. Enforce laws and regulations that protect health and ensure safety
7. Link people to needed personal health services and ensure the provision of health care when otherwise available
8. Ensure a competent public health and personal health care workforce
9. Evaluate effectiveness, accessibility, and quality of personal and population-based health services
10. Research new insights and innovative solutions to health problems
.jpg) Public Health Disease Control/Epidemiology
Public Health Disease Control/Epidemiology
 Public Health (Health Information)
Public Health (Health Information)
 Public Health (Health Promotion)
Public Health (Health Promotion)
 Public Health Evnvironmental Health
Public Health Evnvironmental Health
.jpg)
Session 1: Definition of epidemiology
The word epidemiology comes from the Greek words epi, meaning on or upon, demos, meaning people, and logos, meaning the study of. In other words, the word epidemiology has its origins in the study of what befalls a population. Many definitions have been proposed, but the following definition captures the underlying principles and public health spirit of epidemiology:
"Epidemiology is the study of the distribution and determinants of health-related states or events in specified populations, and the application of this study to the control of heealth problems".
Generally, epidemiology is the study of diseases in given populations. Epidemiologists examine how and where disease outbreaks start, how diseases are transmitted among individuals in a population and how to effectively treat those diseases. The information gathered and analyzed by epidemiologists is then used to develop or improve clinical and medical research, as well as improve preventative healthcare. It’s safe to say that countless lives have been saved due to the work of epidemiologists.
Session 2: Concepts of Disease Occurrence
A critical premise of epidemiology is that disease and other health events do not occur randomly in a population, but are more likely to occur in some members of the population than others because of risk factors that may not be distributed randomly in the population. As noted earlier, one important use of epidemiology is to identify the factors that place some members at greater risk than others.
Disease Causation
A number of models of disease causation have been proposed. Among the simplest of these is the epidemiologic triad or triangle, the traditional model for infectious disease. The triad consists of an external agent, a susceptible host, and an environment that brings the host and agent together. In this model, disease results from the interaction between the agent and the susceptible host in an environment that supports transmission of the agent from a source to that host.
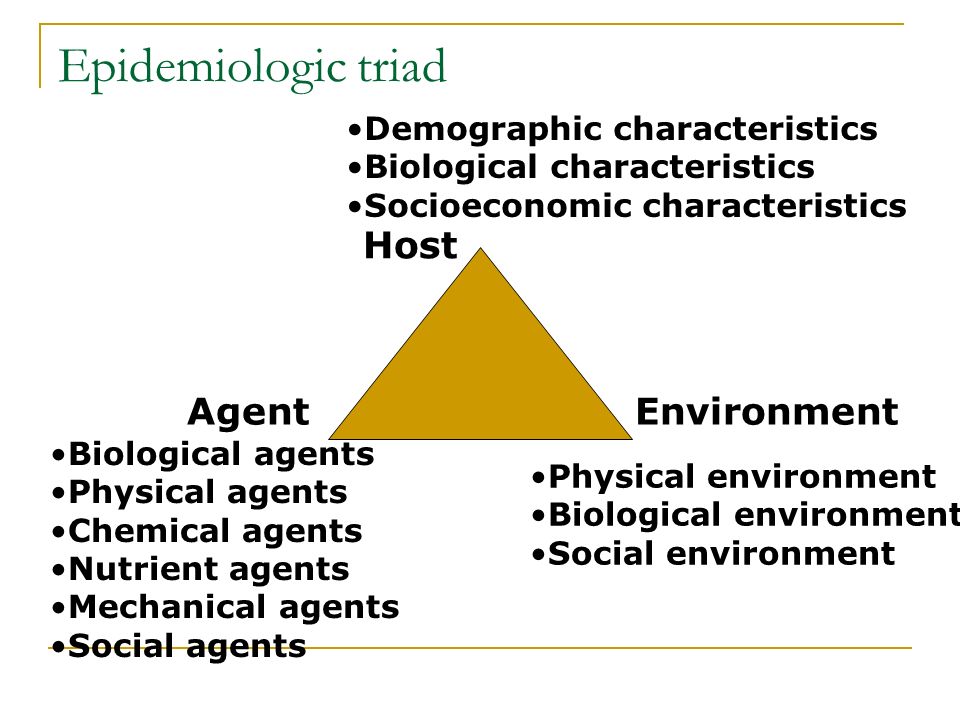
Agent, host, and environmental factors interrelate in a variety of complex ways to produce disease. Different diseases require different balances and interactions of these three components. Development of appropriate, practical, and effective public health measures to control or prevent disease usually requires assessment of all three components and their interactions.
Natural History and Spectrum of Disease
Natural history of disease refers to the progression of a disease process in an individual over time, in the absence of treatment. The process begins with the appropriate exposure to or accumulation of factors sufficient for the disease process to begin in a susceptible host. For an infectious disease, the exposure is a microorganism. For cancer, the exposure may be a factor that initiates the process, such as asbestos fibers or components in tobacco smoke (for lung cancer), or one that promotes the process, such as estrogen (for endometrial cancer).
After the disease process has been triggered, pathological changes then occur without the individual being aware of them. This stage of subclinical disease, extending from the time of exposure to onset of disease symptoms, is usually called the incubation period for infectious diseases, and the latency period for chronic diseases. During this stage, disease is said to be asymptomatic (no symptoms) or in apparent. This period may be as brief as seconds for hypersensitivity and toxic reactions to as long as decades for certain chronic diseases. Even for a single disease, the characteristic incubation period has a range.

What is nutrition?
Nutrition is the science that interprets the interaction of nutrients and other substances in food in relation to maintenance, growth, reproduction, health and disease of an organism. It includes food intake, absorption, assimilation, biosynthesis, catabolism, and excretion.
It can also be defined as molecular biology, biochemistry, and genetics advance, nutrition has become more focused on metabolism and metabolic pathways - biochemical steps through which substances inside us are transformed from one form to another.
Nutrition emphases on how diseases, conditions, and problems can be prevented or reduced with a healthy diet. Also, nutrition involves identifying how certain diseases and conditions may be caused by dietary factors, such as poor diet (malnutrition), food allergies, and food intolerances.
Dietetics Vs Nutrition
Dietetics
Dietetics is the interpretation and communication of the science of nutrition; it helps people make informed and practical choices about food and lifestyle in both health and disease. Part of a dietician's course includes both hospital and community settings. Dietitians work in a variety of areas, from private practice to healthcare, education, corporate wellness, and research, while a much smaller proportion work in the food industry. A dietitian must have a recognized degree or postgraduate degree in nutrition and dietetics and meet continuing education requirements to work as a dietitian.
Nutrition
Nutrition is the study of nutrients in food, how the body uses nutrients, and the relationship between diet, health, and disease.
Why nutrition is important
Eating a balanced diet is vital for good health and wellbeing. Food provides our bodies with the energy, protein, essential fats, vitamins and minerals to live, grow and function properly. We need a wide variety of different foods to provide the right amounts of nutrients for good health. Enjoyment of a healthy diet can also be one of the great cultural pleasures of life. The foods and dietary patterns that promote good nutrition are outlined in the Infant Feeding Guidelines. An unhealthy diet increases the risk of many diet-related diseases.
Nutrition risk factors
The major causes of mortality, morbidity and disability in which diet and nutrition play an important role include coronary heart disease, stroke, hypertension, atherosclerosis, obesity, some forms of cancer, Type 2 diabetes, osteoporosis, dental caries, gall bladder disease, dementia and nutritional anaemia. The Infant Feeding Guidelines help us to eat a healthy diet and help minimize our risk of developing diet-related diseases.

What is the health information?
Health information is the data related to a person's medical history, including symptoms, diagnoses, procedures, and outcomes. Health information records include patient histories, lab results, x-rays, clinical information, and notes. A patient’s health information can be viewed individually, to see how a patient’s health has changed; it can also be viewed as a part of a larger data set to understand how a population’s health has changed, and how medical interventions can change health outcomes.
Understanding Health Information Management
Health information management (HIM) is the practice of acquiring, analyzing, and protecting digital and traditional medical information vital to providing quality patient care. It is a combination of business, science, and information technology.
HIM professionals are highly trained in the latest information management technology applications and understand the workflow in any healthcare provider organization from large hospital systems to the private physician practice. They are vital to the daily operations management of health information and electronic health records (EHRs). They ensure a patient’s health information and records are complete, accurate, and protected.

HIM professionals work on the classification of diseases and treatments to ensure they are standardized for clinical, financial, and legal uses in healthcare. Health information professionals care for patients by caring for their medical data.
HIM professionals are responsible for the quality, integrity, and protection of patient’s health information, which can include any or all of the following:
I. A history and physical exam
II. Lab results—blood tests, urine tests, etc.
III. Clinical information (nursing notes, physical therapy notes, and many others)
IV. X-rays and other radiology procedures and so much more
As technology advances, the role of the HIM professional expands. The HIM professional’s duty is to adapt to new methods of capturing healthcare information, storing that information, and easily accessing it electronically. Their role is important in order to maintain organized and accurate electronic data that allows daily healthcare routines to carry on smoothly with the new technological advancements.

Health information technology (HIT) refers to the framework used to manage health information, and the exchange of health information in a digital format. Professionals who work in HIT are focused on the technical side of managing health information, working with software and hardware used to manage and store patient data. HIT professionals are usually from information technology backgrounds, and provide support for EHRs and other systems HIM professionals use to secure health information. As technology advances, HIT professionals are necessary to ensure the electronic data HIM professionals manage is maintained and exchanged accurately and efficiently.

What is Health Informatics (HI)?
Health Informatics (HI) is a science that defines how health information is technically captured, transmitted, and utilized. Health informatics focuses on information systems, informatics principles, and information technology as it is applied to the continuum of healthcare delivery. It is an integrated discipline with specialty domains that include management science, management engineering principles, healthcare delivery and public health, patient safety, information science and computer technology.
Major Focus Research Areas or Disciplines In Informatics
There are four major focus research areas in informatics education reflecting various disciplines:
I. Medical/Bio Informatics: physician- and research-based; attracts medical students
II. Nursing Informatics: clinical- and research-based; attracts nursing students
III. Public Health Informatics: public health- and bio surveillance-based; attracts public health students
IV. Applied Informatics: addresses the flow of medical information in an electronic environment and covers process, policy and technological solutions; attracts HIM students
Mental health can affect daily life, relationships, and even physical health. Mental health also includes a person's ability to enjoy life - to attain a balance between life activities and efforts to achieve psychological resilience. The positive dimension of mental health is stressed in WHO's definition of health as contained in its constitution: "Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity."
What is Mental Health?
There are several definitions of mental health. Below are few;
According to Medilexicon's medical dictionary, mental health is: "Emotional, behavioral, and social maturity or normality; the absence of a mental or behavioral disorder; a state of psychological well-being in which one has achieved a satisfactory integration of one's instinctual drives acceptable to both oneself and one's social milieu; an appropriate balance of love, work, and leisure pursuits."
According to the World Health Organization, mental health is: "... a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community." The WHO stresses that mental health "is not just the absence of mental disorder."
Ten (10) Facts On Mental Health (WHO, 2018)
Fact 1: Around 20% of the world's children and adolescents have mental disorders or problems.
About half of mental disorders begin before the age of 14. Similar types of disorders are being reported across cultures. Neuropsychiatric disorders are among the leading causes of worldwide disability in young people. Yet most low- and middle-income countries have only one child psychiatrist for every 1 to 4 million people.Fact 2: Mental and substance use disorders are the leading cause of disability worldwide
About 23% of all years lost because of disability is caused by mental and substance use disorders.Fact 3: About 800 000 people commit suicide every year.
Over 800 000 people die due to suicide every year and suicide is the second leading cause of death in 15-29-year-olds. There are indications that for each adult who died of suicide there may have been more than 20 others attempting suicide. 75% of suicides occur in low- and middle-income countries. Mental disorders and harmful use of alcohol contribute to many suicides around the world. Early identification and effective management are key to ensuring that people receive the care they need.Fact 4: War and disasters have a large impact on mental health and psychosocial well-being.
Rates of mental disorder tend to double after emergencies.Fact 5: Mental disorders are important risk factors for other diseases, as well as unintentional and intentional injury.
Mental disorders increase the risk of getting ill from other diseases such as HIV, cardiovascular disease, diabetes, and vice-versa.Fact 6: Stigma and discrimination against patients and families prevent people from seeking mental health care.
Misunderstanding and stigma surrounding mental ill health are widespread. Despite the existence of effective treatments for mental disorders, there is a belief that they are untreatable or that people with mental disorders are difficult, not intelligent, or incapable of making decisions. This stigma can lead to abuse, rejection and isolation and exclude people from health care or support. Within the health system, people are too often treated in institutions which resemble human warehouses rather than places of healing.Fact 7: Human rights violations of people with mental and psychosocial disability are routinely reported in most countries.
These include physical restraint, seclusion and denial of basic needs and privacy. Few countries have a legal framework that adequately protects the rights of people with mental disorders.Fact 8: Globally, there is huge inequity in the distribution of skilled human resources for mental health.
Shortages of psychiatrists, psychiatric nurses, psychologists and social workers are among the main barriers to providing treatment and care in low- and middle-income countries. Low-income countries have 0.05 psychiatrists and 0.42 nurses per 100 000 people. The rate of psychiatrists in high income countries is 170 times greater and for nurses is 70 times greater.Fact 9: There are 5 key barriers to increasing mental health services availability.
In order to increase the availability of mental health services, there are 5 key barriers that need to be overcome: the absence of mental health from the public health agenda and the implications for funding; the current organization of mental health services; lack of integration within primary care; inadequate human resources for mental health; and lack of public mental health leadership.Fact 10: Financial resources to increase services are relatively modest.
Governments, donors and groups representing mental health service users and their families need to work together to increase mental health services, especially in low- and middle-income countries.
What is Mental Illness?
Mental illnesses are diseases or conditions that affect how you think, feel, act, or relate to other people or to your surroundings. Many people have had one or know someone who has. Symptoms can range from mild to severe. They can also vary from person to person. In many cases, it makes daily life hard to handle. But when an expert diagnoses you and helps you get treatment, you can often get your life back on track.
Risk Factors
Specialists say we all have the potential to develop mental health problems, no matter how old we are, whether we are male or female, rich or poor, or which ethnic group we belong to. Almost 1 in 5 experiences mental health problems each year (18.5 percent).
According to WHO, an estimated 9.8 million adults (over 18) had a serious mental disorder in the United States in 2015. That equates to 4.8 percent of all American adults. A large proportion of the people who have a mental disorder have more than one. Also in the U.S. and much of the developed world, mental disorders are one of the leading causes of disability [1]
Common Mental Disorders
There are several mental disorders, however, the most common types of mental illness are anxiety disorders, mood disorders, and schizophrenia disorders; beneath we explain each in turn:
>> Anxiety disorders
Anxiety disorders are the most common type of mental illness.
The individual has a severe fear or anxiety, which is linked to certain objects or situations. Most people with an anxiety disorder will try to avoid exposure to whatever triggers their anxiety. Examples of anxiety disorders include:
I. Panic disorder - the person experiences sudden paralyzing terror or a sense of imminent disaster.
II. Phobias - these may include simple phobias (a disproportionate fear of objects), social phobias (fear of being subject to the judgment of others), and agoraphobia (dread of situations where getting away or breaking free may be difficult). We really do not know how many phobias there are - there could be thousands of types.
III. Obsessive-compulsive disorder (OCD) - the person has obsessions and compulsions. In other words, constant stressful thoughts (obsessions), and a powerful urge to perform repetitive acts, such as hand washing (compulsion).
IV. Post-traumatic stress disorder (PTSD) - this can occur after somebody has been through a traumatic event - something horrible or frightening that they experienced or witnessed. During this type of event, the person thinks that their life or other people's lives are in danger. They may feel afraid or feel that they have no control over what is happening.
>> Mood disorders
These are also known as affective disorders or depressive disorders. Patients with these conditions have significant changes in mood, generally involving either mania (elation) or depression. Examples of mood disorders include:
I. Major depression - the individual is no longer interested in and does not enjoy activities and events that they previously liked. There are extreme or prolonged periods of sadness.
II. Bipolar disorder - previously known as manic-depressive illness, or manic depression. The individual switches from episodes of euphoria (mania) to depression (despair).
III. Persistent depressive disorder - previously known as dysthymia, this is mild chronic (long term) depression. The patient has similar symptoms to major depression but to a lesser extent.
IV. SAD (seasonal affective disorder) - a type of major depression that is triggered by lack of daylight. It is most common in countries far from the equator during late autumn, winter, and early spring. Read more on SAD
>> Schizophrenia disorders
Whether or not schizophrenia is a single disorder or a group of related illnesses has yet to be fully determined. It is a highly complex condition. Schizophrenia normally begins between the ages of 15 and 25. The individual has thoughts that appear fragmented; they also find it hard to process information.
Schizophrenia has negative and positive symptoms. Positive symptoms include delusions, thought disorders, and hallucinations. Negative symptoms include withdrawal, lack of motivation, and a flat or inappropriate mood. (Read further "What is schizophrenia")
Early Signs Of Mental Disorders
It is not possible to reliably tell whether someone is developing a mental health problem; however, if certain signs appear in a short space of time, it may offer clues of:
I. Withdrawing from people or activities they would normally enjoy.
II. Sleeping or eating too much or too little.
III. Feeling as if nothing matters.
IV. Consistently low energy.
V. Using drugs more than normal (including alcohol and nicotine).
VI. Displaying uncharacteristic emotions.
VII. Confusion.
VIII. Not being able to complete standard tasks, such as getting to work or cooking a meal.
IX. Persistent thoughts or memories that reappear regularly.
X. Thinking of harming one's self or others.
XI. Hearing voices.
XII. Delusions.
^^ Treatment ^^
It is important to know that what works for one person may not work for another; this is especially the case with mental health. Some strategies or treatments are more successful when combined with others. A patient with a chronic mental disorder may choose different options at different stages in their life. The majority of experts say that a well-informed patient is probably the best judge of what treatment suits them best. However, treatment may include: Psychotherapy (talking therapies) , Medication, and Self-help.
Doctor's suicide rate highest of any profession
Doctors who die by suicide often have untreated or undertreated depression or other mental illnesses, a fact that underscores the need for early diagnosis and treatment. Read full article
"Mental Health Quotes"
There is no health without mental health; mental health is too important to be left to the professionals alone, and mental health is everyone's business (By Vikram Patel)
A child's mental health is just as important as their physical health and deserves the same quality of support. Together with open conversations and greater understanding, we can ensure that attitudes for mental health change and children recieve the support they deserve (By Kate Middleton)
People talk about physical fitness, but mental health is equally important. I see people suffering, and their families feel a sense of shame about it, which dosen't help. One needs support and understanding. I am now working on an initiative to create awareness about anxiety and depression and help people (By Deepika Padukone)

Health promotion is defined as "any planned combination of educational, political, environmental, regulatory, or organizational mechanisms that support actions and conditions of living beneficial to the health of individuals, groups, and communities". Health promotion can take account of interventions on multiples levels from public policy to teaching individuals, and addresses areas such as health behavior change, social determinants of health and health literacy.
Health Promotion Actions
1. Health Promotion Action #1: Build healthy public policy
2. Health Promotion Action #2: Create supportive environments
3. Health Promotion Action #3: Strengthen community actions
4. Health Promotion Action #4: Develop personal skills
5. Health Promotion Action #5: Re-orient health services
Purpose Of Health Promotion
The purpose of health promotion is to positively influence the health behavior of individuals and communities as well as the living and working conditions that influence their health.
Why Health promotion?
1. Health promotion improves the health status of individuals, families, communities, states, and the nation.
2. Health promotion enhances the quality of life for all people.
3. Health promotion reduces premature deaths.
4. By focusing on prevention, health promotion reduces the costs (both financial and human) that individuals, employers, families, insurance companies, medical facilities, communities, the state and the nation would spend on medical treatment.
Theories and Models of Health Promotion and Disease Prevention
There are more than a few theories and models that support the practice of health promotion and disease prevention. Theories and models are used in program planning to understand and explain health behavior and to guide the identification, development, and implementation of interventions.
Before ascertaining a theory or model to guide health promotion and disease prevention programs, it is imperative to consider a range of dynamics, for instance the specific health problem being addressed, the people being served, and the contexts within which the program is being implemented. Health promotion and disease prevention programs characteristically draw from one or more theories or models.
Beneath are selected theories and models that are used for health promotion and disease prevention programs:
1. Ecological Models
2. The Health Belief Model
3. Stages of Change Model
4. Social Cognitive Theory
5. Theory of Reasoned Action/Planned Behavior
Jobs Directly Related to Health Promotion Include:
Community development worker.
Further education teacher.
Health promotion specialist.
Health service manager.
Medical sales representative.

Definition of Environmental Health
Environmental Health is the field of science that studies how the environment influences human health and disease. In the context of environmental health, “Environment,” means things in the natural environment like air, water and soil, and also all the physical, chemical, biological and social features of our surroundings.
The man-made environment includes physical structures where people live and work such as homes, offices, schools, farms and factories, as well as community systems such as roads and transportation systems, land use practices and waste management. Consequences of human alteration to the natural environment, such as air pollution, are also parts of the man-made environment. The social environment encompasses lifestyle factors such as diet and exercise, socioeconomic status, and other societal influences that may affect health. – National Institute of Environmental Health Science
Goal
Promote health for all through a healthy environment
Why Is Environmental Health Important?
Maintaining a healthy environment is central to increasing quality of life and years of healthy life. Globally, 23% of all deaths and 26% of deaths among children under age 5 are due to preventable environmental factors (WHO, 2016). Poor environmental quality has its greatest impact on people whose health status is already at risk. Therefore, environmental health must address the societal and environmental factors that increase the likelihood of exposure and disease. Environmental factors are diverse and far reaching. They include:
i) Exposure to hazardous substances in the air, water, soil, and food
ii) Natural and technological disasters
iii) Climate change
iv) Occupational hazards
v) The built environment
Emerging Issues in Environmental Health
Environmental health is a dynamic and sprouting field. While not all complex environmental issues can be predicted, some known emerging issues in the field include: climate change, disaster preparedness, nanotechnology, the built environment, exposure to unknown hazards and blood lead levels.
Environmental Disease
In epidemiology, environmental diseases are diseases that can be directly attributed to environmental factors (as different from genetic factors or infection). If a disease process is concluded to be the result of a combination of genetic and environmental factor influences, its etiological origin can be referred to as having a multifactorial pattern.
Environmental Hazard
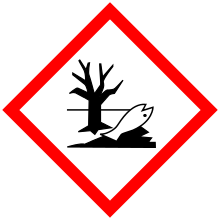
An environmental hazard is a substance, a state or an event which has the potential to threaten the surrounding natural environment or adversely affect people's health, including pollution and natural disasters such as storms and earthquakes. The hazard can be of toxic chemical, biological, or physical agents in the environment, resulting from human activities or natural processes, that may impact the health of exposed subjects, including pollutants such as heavy metals, pesticides, biological contaminants, toxic waste, industrial and home chemicals
Human-made hazards while not immediately health-threatening may turn out detrimental to man's well-being eventually, because deterioration in the environment can produce secondary, unwanted negative effects on the human ecosphere. Likewise, the effects of water pollution may not be immediately visible because of a sewage system that helps drain off toxic substances.
Categorization or types of hazards
1. Chemical
2. Physical (mechanical)
3. Biological
4. Psychosocial
How You Can Create a Healing Environment at Home
Beneath are some ways to do that;
Go for comfort, Cut the clutter, Delight your senses, Enhance the light, Bring nature in, Reduce the roar, Don’t forget the garden, Start small and Consider your inner environment.

Session 1: Introduction to First Aid
What is First Aid?
First Aid is an immediate care given to an injured or suddenly ill person without any proper medical equipment. It is a temporary assistance until arrival of competent medical care and does not take the place of proper medical treatment.
What is the importance of First Aid?
First Aid can sometimes save life such as choking, cardiac arrest and during accidents.
Who should provide First Aid and where should Who should provide First Aid be provided?
EVERYBODY, All health personnel, Especially Professional Health Personnel and Most especially YOU. First Aid can be provided EVERYWHERE.
Aims of First Aid (3P’s)
1. To preserve life
2. To protect the casualty from further harm
3. To promote recovery
Principles of First Aid
1st Principle: Do no harm; know what to do and know what NOT to do
2nd Principle: First aid is NOT an exact science and is open to error
3rd Principle: First Aid is about Putting First Things First, thus:
i. Get your priority right: know and recognize what is an emergency and what is not an emergency
ii. If there are too many cases, treat the most urgent first
iii. If there are too many casualties, first call for help and then treat the ones with the highest chance of survival
4th Principle: Safety is very important in first aid, however, always:
i. Check for danger
ii. Assess the scene by: Evaluating and assessing safety of the scene, prioritize care and check for medical alert tags. Also, do head-to-toe check and move only if necessary.
Seven essential First Aid Interventions
1. Call for ambulance
2. DO NOT move and DO NOT allow movement unnecessarily of a trauma casualty
3. Perform chin lift or head tilt chin lift
4. Mouth-to-mouth breathing (if willing) especially in children, drowning or poisoning
5. Chest compression
6. Operate an automated external defibrillator
7. Stop any bleeding
Session 2: First Aid Preliminary Actions (Click here to download)
Session 3: Cardiopulmonary Resuscitation (CPR) (Click here to download)
Session 4: Defibrillation (AED) (Click here to download)
Session 5: Secondary Assessment (Click here to download)
Session 6: Foreign Body Airway Obstruction (FBAO) (Click here to download)
Session 7: Bleeding (Click here to download)
Session 8: Fractures (Click here to download)
Session 9: Concussion (Click here to download)
Session 10: Head Injury (Click here to download)
Session 11: Soft Tissue Injury (Click here to download)
Session 12: Spinal Injury (Click here to download)
Session 13: Sucking Chest Wound (Click here to download)
Session 14: Burns (Click here to download)
Session 15: Diabetes Emergencies (Click here to download)
Session 16: Emergency Childbirth (Click here to download)
Session 17: Poisoning (Click here to download)
Session 18: Seizures (Click here to download)
Session 19: Snake bite (Click here to download)
Session 20: Legal aspects of First Aid (Click here to download)

KEY POINTS TO REMEMBER
Medical emergencies can happen anytime. Hence, act quickly, calmly, correctly and consider being certified in first aid and CPR.
"Whatever can happen to one man can happen to every man.”
Lucius Annaeus Seneca (4 B.C.? – A.D.65)
Further Reading on Public Health Disciplines
Principles of Epidemiology In Public Health Practice ( Click here to download )
Expanded Programme on Immunization Field Guide ( Click here to download )
Technical Guidelines Integrated Disease Surveillance and Response Ghana, 2nd Edition ( Click here to download )
Health promotion action (Read more)
Infant Feeding Guidelines ( Click here to download )
Theory and Fundamentals of Health Promotion for Children and Adolescents ( Click here to download )
Theories and Models Frequently Used in Health Promotion ( Click here to download )
The Health Promotion Strategic Framework ( Click here to download )
Effects of deforestation on public health (Read more)
Environmental medicine (Read more)
Mental Health (Read more about mental disorders)
Mental disorders linked by genetics traits (Read more)
References
Gold, Robert S.; Miner, Kathleen R. (2002). "Report of the 2000 Joint Committee on Health Education and Promotion Terminology". Journal of School Health. Wiley-Blackwell. 72 (1): 3–7. doi:10.1111/j.1746-1561. 2002.tb06501. x. ISSN 0022-4391.
World Health Organization (2006). Preventing disease through healthy environments. Geneva, Switzerland.
Patz J, et al. (2005). Impact of regional climate change on human health. Nature; 438(7066):310-17.
Kinney PL. (2008). Climate change, air quality, and human health. Am J Prev Med;35(5):459-67.
Environmental hazard(2014). Defined Term - A dictionary of legal, industry-specific, and uncommon terms. Quoted from Code of Maryland. https://en.wikipedia.org/wiki/Environmental_hazard#cite_ref-1
National Institute of Mental Health (2016). Serous mental illness (SMA) among U.S. adults.
National Institute of Mental Health (2013). U.S. leading categorties of diseases/disorders.